Hepatitis C is a viral infection that affects the liver, one of the body’s most vital organs. Unlike some illnesses that show clear symptoms early on, hepatitis C often progresses silently, making early detection essential for protecting long-term health. Millions of people around the world live with this infection without realizing it, and by the time symptoms appear, the liver may already have sustained significant damage. Understanding the importance of early diagnosis, along with prevention and treatment options, can make the difference between a manageable condition and life-threatening complications.
What is hepatitis C?
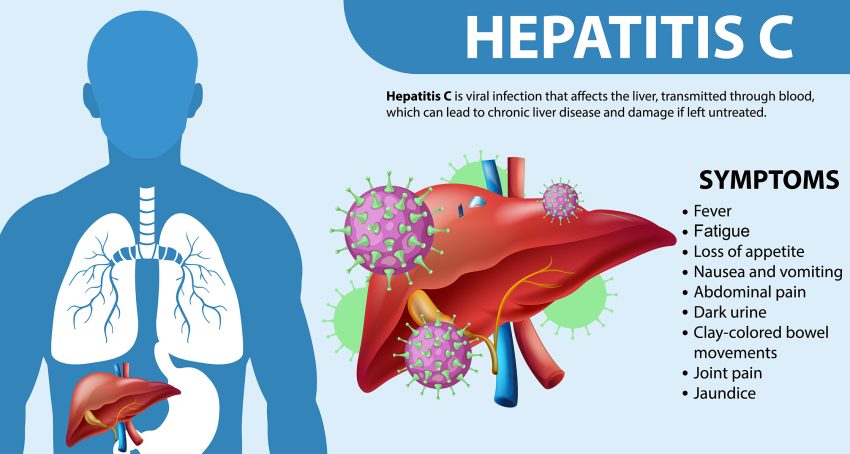
Hepatitis C is caused by the hepatitis C virus (HCV), which primarily spreads through blood-to-blood contact. It can result in both acute and chronic infections. Acute hepatitis C refers to the first six months after exposure, when some people may clear the virus naturally. However, in most cases, the infection becomes chronic, meaning it remains in the body long-term and can damage the liver over time.
Chronic hepatitis C is particularly dangerous because it often develops quietly, without noticeable symptoms, until advanced liver disease sets in. This silent progression is one of the main reasons early detection is so important.
How hepatitis C spreads
The virus spreads when infected blood enters another person’s bloodstream. The most common routes include:
- Sharing needles, syringes, or other equipment for injecting drugs
- Receiving blood transfusions or organ transplants before widespread screening began (in many countries, this was before 1992)
- Exposure through unsafe medical practices or improperly sterilized equipment
- Occupational exposure in healthcare settings
- Rarely, through sexual contact or from mother to child during childbirth
Understanding these risk factors is the first step toward both prevention and timely testing.
Why early detection is critical
Preventing liver damage
Hepatitis C primarily attacks the liver. Over time, chronic infection can lead to scarring (fibrosis), severe scarring (cirrhosis), and eventually liver cancer or liver failure. These complications may take years or even decades to develop, but once advanced damage occurs, treatment options are limited and more complicated. Detecting the virus early allows for timely treatment that can prevent long-term liver damage.
Protecting others
Because many people are unaware they carry the virus, hepatitis C continues to spread silently. Identifying and treating infected individuals reduces the risk of unknowingly transmitting the virus to others, whether through medical procedures, drug use, or other blood-related exposures. Early detection is therefore not only about individual health but also about public health.
Access to highly effective treatments
In recent years, medical advances have transformed hepatitis C treatment. Direct-acting antiviral (DAA) medications can cure more than 95% of patients, usually with just 8 to 12 weeks of therapy. However, to benefit from these treatments, a person must first be diagnosed. Without testing, individuals may live for years unaware of a treatable and curable infection.
Signs and symptoms to watch for
Although hepatitis C is often asymptomatic in its early stages, some people may experience mild or vague symptoms such as fatigue, loss of appetite, joint pain, or abdominal discomfort. In advanced stages, signs like jaundice (yellowing of the skin and eyes), swelling in the legs, or confusion due to liver malfunction may appear. These late symptoms often indicate serious liver damage, reinforcing why testing is vital even without obvious signs of illness.
Who should get tested?
Health organizations worldwide recommend hepatitis C testing for certain groups:
- People who have ever injected drugs, even once
- Those who received blood transfusions or organ transplants before 1992
- Individuals on long-term hemodialysis
- Healthcare workers exposed to blood through accidents
- People living with HIV
- Anyone with abnormal liver enzyme tests without a clear cause
- Adults born between 1945 and 1965 (in some countries, this age group shows higher infection rates)
Routine one-time screening is increasingly encouraged for all adults, as risk factors alone may not always identify every case.
How hepatitis C is diagnosed
Testing for hepatitis C usually begins with a simple blood test that checks for antibodies to the virus. A positive antibody test means a person has been exposed to HCV at some point. To confirm an active infection, another test detects the virus’s genetic material (RNA) in the blood. These tests are widely available, relatively inexpensive, and provide essential information for starting treatment.
Treatment and management after early detection
Once diagnosed, treatment decisions depend on the stage of liver disease, the specific strain of the virus, and other health factors. Modern antiviral therapies are highly effective, with minimal side effects compared to older treatments. Most people can expect a full cure, meaning the virus is no longer detectable in the blood.
Early treatment not only protects the liver but also improves overall health and quality of life. Patients who achieve a cure have reduced risks of cirrhosis, liver cancer, and other complications. For those already living with liver damage, early medical intervention helps slow disease progression and provides better long-term outcomes.
The cost of delayed diagnosis
Delaying diagnosis can lead to advanced liver disease, which is much harder and more expensive to treat. Cirrhosis may require liver transplantation, a complex and costly procedure with significant risks. Furthermore, untreated hepatitis C increases healthcare costs for both individuals and healthcare systems, while also leading to unnecessary suffering. By contrast, early detection and timely treatment offer a cost-effective solution with excellent success rates.
Practical steps for prevention
While treatment cures the infection, prevention remains crucial. Simple practices can significantly reduce the risk of hepatitis C transmission:
- Avoid sharing needles, syringes, or personal items like razors and toothbrushes
- Ensure medical and dental procedures use properly sterilized equipment
- Practice safe sex if at higher risk of blood exposure
- Regularly test if you fall into a high-risk group
- Seek professional care immediately if exposed to potentially infected blood
These preventive steps, combined with widespread awareness, are key to reducing hepatitis C cases worldwide.
Looking ahead: building a future free of hepatitis C
Global health organizations, including the World Health Organization, have set ambitious targets to eliminate hepatitis C as a public health threat in the coming decades. Early detection, accessible treatment, and effective prevention strategies are the pillars of this goal. Every person who gets tested and treated brings the world one step closer to eliminating the disease.
The message is clear: hepatitis C is curable, but only if it is found. By encouraging regular screening, raising awareness, and supporting preventive measures, individuals and communities can work together to stop the silent damage of this virus. The earlier hepatitis C is detected, the greater the chance of protecting both liver health and overall well-being.